We use cookies on this website. By using this site, you agree that we may store and access cookies on your device. Find out more.
Obituaries
Amber Elizabeth Young
 Amber Elizabeth Young
Amber Elizabeth Young
Consultant paediatric anaesthetist and professor of burns care, University of Bristol 1963-2022
(b 1963; q Bristol, 1987; PhD, FRCA),
Died from breast cancer on 17 September 2022
Also available : BMJ Obituary https://doi.org/10.1136/bmj.o2618
I am honoured to be asked to give a tribute to Professor Amber Young who sadly died of breast cancer in September. Amber was an absolutely extraordinary person in so many aspects of her life and this could so easily just be a list of exalted titles and onerous responsibilities that she carried and lived up to.
Amber was appointed as a consultant paediatric anaesthetist at Frenchay Hospital, Bristol in 1991. Not long after her arrival, she set to work building up the paediatric service, Amber subspecialised in the challenging fields of children’s burns care and neurosurgical care. She published extensively and literally set out to change the world of Paediatric Burn care, which she did.
Amber had a prolific career in paediatric burns clinical care and research - she was chair of the British Burn Association, chair of NHS England burns clinical reference group, Network lead for Southwest paediatric burns and was working with The Healing Foundation and Scar Free Foundation. She forged links with Bristol, Bath and Cardiff universities as she developed her burns research career pathway. Amber did all of this with little fanfare and at times was also managing cancer treatments around her work schedule.
I first met Amber as an anaesthetic registrar in 2003, and to start with I knew little about her except she was leading a service that provided excellent care for sick children and whenever a daunting paediatric emergency arose, she would be there to help and to guide. As I got to know her better, I was inspired by her meticulous approach to perioperative paediatric care and obvious passion for the job and I was encouraged to train in the same field and eventually proudly joined the small team of paediatric anaethetists at Frenchay Hospital.
I learnt so much in those early consultant years from Amber - she was a brilliant clinician, and leader, skilful and methodical in her approach, she was able to teach the detail of how to handle a high-risk situation. There are a great many things I still do now, exactly the same way as she taught me, I have not found a way to improve upon them. Amber was devoted to the care of sick children, she set extremely high standards, which inspired the rest of us to do the same.
Amber was a very private and dignified person she was first diagnosed with breast cancer in 2006, she maintained drive and determination and scheduled meetings and lists around her treatment regime. In 2014 Paediatric services were centralised to Bristol Children’s Hospital and Amber was also key in the planning and implementation of this project too. Sadly, in 2016 Amber’s breast cancer returned, but this made her even more determined to continue and complete vital paediatric burns research, unfortunately she was not able to continue with clinical work (peripheral neuropathy from the chemo made it too tricky to cannulate reliably but I do recall she did help with a line and was of course successful!) Amber completed a PhD, delivered the Wallace Memorial Lecture at the British Burn Association in 2018 and was awarded the position of Professor of paediatric burn care by Bristol University in the summer - that was one of the happiest conversations we had had, Amber was very content and said “it doesn’t really change anything, but I am so happy - good news for once!”
Aside from Amber’s many talents at work Amber was also an extremely kind and generous friend, mentor and an amazing cook. She and her husband Norman created a beautiful home together and were fabulous hosts. Many of us looked forward to their Christmas parties – they were wonderful occasions and brought their local community together.
Amber will be very much missed by all her friends and colleagues; I think of her often.
Natasha Clark
Consultant Paediatric Anaesthetist
Bristol
The following text has been taken from the BMJ Obituary
Amber Elizabeth Young was the eldest of three children born to Patricia, a nurse, and John, a consultant psychiatrist. She excelled at school and came to Bristol to read medicine in 1981. She graduated in 1987, also having gained an intercalated BSc in biochemistry. Declaring a paediatric interest early in her postgraduate training, she undertook anaesthetic training on the south-west anaesthetic rotation and was appointed consultant paediatric anaesthetist at Frenchay Hospital in 1999.
Amber made her presence felt immediately, as a sound clinical opinion and a superb anaesthetist. In 2001 Frenchay won the Hospital Doctor award for the “best paediatric team” under her leadership. She was instrumental in supporting children’s acute care facilities at Frenchay, which proved essential in allowing the development of the nascent paediatric neurosurgical and burns services on that site.
Forever a vocal advocate for her patients and colleagues, she took a leading role in managing the complex project required to move her beloved services safely to Bristol children’s hospital in 2014.
As multitalented as she was, Amber’s interests eventually gravitated towards research in children’s burns, and she became increasingly active in that area. Becoming first a regional, then national and finally an international authority, all in a remarkably brief period of time.
Treatment for breast cancer, first diagnosed in 2006, didn’t noticeably slow her down, and she went on to gain first a PhD, the presidency of the British Burns association, and then appointment as professor at the university of Bristol, not to mention acquiring several NHIR research fellowships along the way—all this while undergoing chemotherapy.
Despite her dedication to children’s burns research, Amber was also talented paediatric neuro-anaesthetist and under her stewardship, paediatric neurosurgery in Bristol achieved national designation in epilepsy, spasticity, and craniofacial surgery. That we are now a department of major national and international repute is very much down to the support she gave us in those early years.
I shall remember Amber as an ever industrious, relentlessly enthusiastic colleague and a wonderfully supportive, kind, and humorous friend. I shall remember sitting in her kitchen drinking wine, and all her madcap domestic projects, often involving craning impossibly heavy stone ornaments into her tiny garden in Clifton.
The stars aligned for her in 2012 when she met and married her soulmate, Norman. Together they wove a story of love and contentment, building themselves a lovely home in rural Somerset, where for many years they laughed, entertained, and planned spectacular holidays abroad.
With her illness came a wiser, gentler acceptance of the human condition and the fragility of everything. And of what really mattered, which for Amber, was those that she loved and the time she spent with them.
It was the greatest pleasure to have known and worked with Amber. She made a huge difference to the lives of countless sick children and to her many friends and colleagues worldwide.
She leaves her mother; siblings; niece and nephews; and her beloved husband Norman.
We will miss her terribly and think of her often.
Consultant paediatric anaesthetist and professor of burns care, University of Bristol (b 1963; q Bristol, 1987; PhD, FRCA), died from breast cancer on 17 September 2022
Gerry Black
Dr Gerry Black of Belfast (APA President 1985 - 87) passed away on Wednesday 10th July 2019.
Kester Brown

We have been deeply saddened to hear of the passing of Dr Kester Brown.
Kester was a giant in the world of paediatric anaesthesia with a global network of people he had supported and mentored.
Tony Nightingale
It is with great sadness that we must report the loss of Dr Tony Nightingale who was one of the early prominent figures of paediatric anaesthesia, and indeed one of the founder members of the APAGBI.
He was a true gentleman with many accomplishments to his name. He was a great advocate of trainees and training and created opportunities for British trainees and also promising overseas trainees to work at Alder Hey as part of a rotation. He was also a great supporter of ODPs. He was involved in research and also the creation of some of the early standards fort paediatric anaesthesia which were used nationally and internationally.
He was streets ahead of Great Thunberg and was forever preaching “reduce, reuse, recycle” for all anaesthetic equipment.
And very touchingly, at Christmas he would always arrive with boxes of satsumas for the staff of the various depts with whom he was involved. A tradition which has been continued since his retirement.
An all round gentleman who will be missed greatly.
Gerry Black
Dr Gerry Black of Belfast (APA President 1985 - 87) passed away on Wednesday 10th July 2019.
Kester Brown

We have been deeply saddened to hear of the passing of Dr Kester Brown.
Kester was a giant in the world of paediatric anaesthesia with a global network of people he had supported and mentored.
Vale Robert Eyres

Robert Eyres was an Honorary Member of the APAGBI, a Nuffield prize winner and an inspirational member of the department in Melbourne.
Rob came from Deniliquin, NSW and was educated at Caulfield Grammar School and Melbourne University. His training in Anaesthesia was undertaken at Whipps Cross Hospital in London. He won the prize in the final FFARCS examinations. He returned to Melbourne in 1977 and worked as a registrar at the Royal Children’s Hospital. The following year he joined the full time staff. For many years he worked one night a week in Intensive Care. He remained on staff at RCH for 40 years.
He soon took charge of cardiac anaesthesia. He led the research program on blood levels of local anaesthetics in children (first in the world) and helped to establish epidural anaesthesia in the hospital. He was a very competent practical anaesthetist. He had a brilliant mind and could get to the nub of a problem quickly and was able to explain things clearly and concisely. He was a highly regarded teacher.
He undertook a sabbatical in Italy and often went to France for holidays.
In 2000-2004 he was Director of Anaesthesia at the Royal Children’s Hospital. This included a time as Director of Specialist Services.
Rob was heavily involved with SPANZA including role as treasurer. In 2008 he was awarded the SPANZA medal and conferred Honorary Life membership.
Rob will be fondly remembered for his love of people, fast cars, fast bikes and red wine.
Like his signature boots Rob’s life was well worn and well loved.
“Life’s too short to drink white”
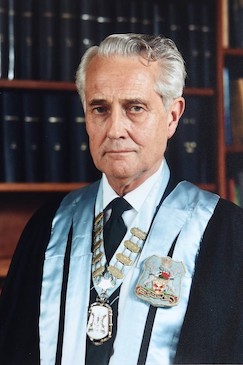
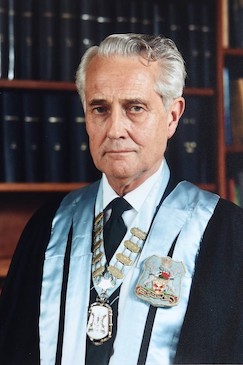
Gordon Henry Bush

Dr Gordon Henry Bush was recognised as a leading paediatric anaesthetist the world over; asked to describe him, friends and colleagues invariably begin ‘He was a real Gentleman…’
Roddy McNicol

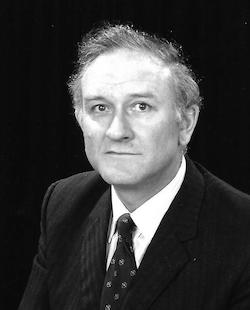
It is with great sadness that I write this tribute to my friend and office-buddy of some 25 years Roddie McNicol who has died suddenly on 5th December 2016 in France at the age of 71 years.
Roddie was educated at Allan Glens School and the University of Glasgow. He trained in anaesthesia in Glasgow and was appointed as a Consultant with clinical sessions mainly in orthopaedics, plastic surgery and paediatrics. He was co-author of one of the first papers on ketamine pharmacokinetics in children in 1983 and with Douglas Arthur wrote a very influential review of local anaesthetic techniques in children for the British Journal of Anaesthesia in 1986. This, along with his many lectures, tutorials and one-to-one clinical teaching sessions, encouraged widespread adoption of regional anaesthesia in paediatric practice. Here Roddie is seen in typical pose, sharing an anecdote with Jack Rees.
John Keneally

John Keneally was one of the doyens of Australian paediatric anaesthetic practice, but with true modesty he would have been the last to have accepted this. Nevertheless, JK – as he was lovingly known – touched the lives and careers of many hundreds of anaesthetic trainees, as they passed through the Royal Alexandra Hospital for Children and thousands of anaesthetists through his contributions to anaesthetic literature and journalism.
Edward Battersby

Edward Fletcher Battersby (“Ted”) was brought up in Christchurch, New Zealand. After qualifying at the University of Otago he was a houseman in Christchurch before working his passage to England as a ship’s doctor. He then undertook junior posts at Bart’s and Great Ormond Street, going back to New Zealand in 1962. He returned to England to settle permanently in 1964, where he was appointed as a consultant at Great Ormond Street.
John Inkster

John Inkster, who has died aged 87, was a pioneer in anaesthesia and intensive care techniques that helped to make complex surgery safer for small babies.
Professor A. W. Conn
Professor Alan William Conn died 2nd October 2010. 'Al' was born on May 29 1925 at Mimico, Ontario, Canada where his father was a General Practitioner and he graduated MD from the University of Toronto in 1948.
Bill Glover
William John Glover MB, BCh, BAO, FRCA
Bill Glover was the first full time paediatric anaesthetist to be appointed at Great Ormond Street Children’s Hospital in London. He was a key figure in the establishment of mechanical ventilation of children in the hospital and in obtaining recognition for anaesthetists as equal colleagues by the medical staff.
Dr William John Glover was born in Crosscar, Northern Ireland on 20th May 1927, the fifth of six children. His father was a farmer. He was educated at the local church Primary School and at Down High School, Downpatrick, County Down, and qualified MB, ChB, BAO from Queen’s University Belfast in 1950. He held House Officer appointments at The Royal Victoria Hospital, Belfast, The Royal Belfast Hospital for Sick Children and Hull Maternity Hospital, obtaining the D.Obst.RCOG in 1953. After three years in General Practice in Plymouth he returned to Belfast to begin his anaesthetic training as an SHO, followed by registrar appointments at Manchester Royal Infirmary and Great Ormond Street (GOS). He completed his anaesthetic training as Senior Anaesthetic registrar on the Manchester rotation from 1957 to 1959 and was appointed part-time (5 sessions) consultant paediatric anaesthetist at GOS in 1960. Following a year as a Fellow in anesthesiology at the Mayo Clinic in Rochester, Minnesota, he returned to GOS and also obtained a 2 session consultant appointment at the Eastman Dental Hospital before becoming GOS’s first full-time paediatric anaesthetist in 1963. Previously the anaesthetic department had been staffed on a sessional basis by part-time consultants with commitments at London teaching hospitals and in private practice. Most of the anaesthesia for emergency and ‘out of hours’ surgery was provided by two senior registrars and four or five registrars.
Bill was appointed at a time when paediatric cardiac surgery was in its infancy, developing under the leadership of surgeons David Waterston and Eoin Aberdeen, and cardiologist Dick Bonham Carter. Much of the early surgery was palliative and operations such as banding of the pulmonary artery led to postoperative respiratory insufficiency, sometimes requiring ventilatory support for periods of months or occasionally years. Bill resurrected a couple of Engstrom 160 ventilators which were in storage at GOS following the poliomyelitis days, and purchased others from Sweden, with advice from Dr Alvar Swenson, Head of paediatric anaesthesia at the Karolinska Institute in Stockholm. He thus established, with help from GOS’s second paediatric anaesthetist, Ted Battersby, one of the world’s first paediatric respiratory care units, a forerunner of today’s paediatric intensive care units. He later helped to pioneer anaesthesia for paediatric craniofacial surgery.
Bill soon established a reputation not only as a dedicated paediatric anaesthetist but also as a wise counsel at the Medical Staff Committee, which at that time virtually ran the hospital, and a superb administrator. It was largely due to his influence that anaesthetists, who had previously not been invited to sit on the Medical Staff Committee, were recognised as equals by the GOS medical establishment. He served on numerous committees, including the Board of Governors, later the Special Health Authority, becoming Vice-Chairman of both under Audrey Callaghan’s chairmanship from 1974 to 1990. Outside GOS he was a staunch supporter of the Royal Society of Medicine, serving on the committee of the section of anaesthetics from 1962-65, and subsequently being elected a life member. He also became a life member of the British Medical Association after having been a member for 50 years. From 1965-80 he served on the anaesthetic sub-group of the British Standards Institute. Although primarily a clinical anaesthetist his lectures and writings were always informative and delivered with his usual succinct clarity. He retired at the age of 65 in 1992.
In the early 1970’s communication between anaesthetists in the large paediatric centres in the UK was scant or non-existent and in order to improve the situation Bill was a keen supporter of the establishment of the Association of Paediatric Anaesthetists, becoming a founder member in 1973 and President from 1989-1991. Along with other founder members, he firmly believed that the aims of the Association would be best met by restricting membership to those whose main interest was paediatric anaesthesia and who could learn from each other’s advances and well as their mistakes in the informal atmosphere created at the annual meeting by a relatively small group. His fear, which I confess I shared, was that opening membership to the large number of anaesthetists whose work occasionally involved children, many of whom were anxious to join, would fundamentally change the nature of the Association and inhibit this frank exchange of views. This view prevailed for several years despite accusations of elitism, but pressure from the anaesthetic fraternity eventually led to the opening of membership to virtually anyone who wished to join.
This tribute would not be complete without a brief personal reflection on Bill, with whom I worked as a colleague for over twenty years. He had a warm and unassuming nature, was always approachable, and his advice was invariably sound and well thought through. He had an amazing memory and attention to detail, and a shrewd knack of quickly getting to the heart of any problem. It was never wise to seek his advice without being fully briefed about the situation presented to him. Keenly interested in promoting the careers and welfare of the trainee members of the department, he encouraged me to follow in his footsteps as a Fellow at the Mayo Clinic, which gave me the experience of cardiac anaesthesia necessary for a consultant post at GOS. Later he encouraged me to apply for election to the council of both the Association of Anaesthetists and later the then Faculty of Anaesthetists of the Royal College of Surgeons, despite the extra clinical workload which he knew such appointments would place on him. It was a privilege to have been both a colleague and friend.
Bill Glover died on 30th October 2019. He leaves a wife, Raye, three children and eight grandchildren.
David Hatch


